 This post may be one of those posts which may be picked up by larger organizations and cited a lot more than others. I am also very certain that this post will be more likely to get attacked and commented on due to the nature of a post like this.
This post may be one of those posts which may be picked up by larger organizations and cited a lot more than others. I am also very certain that this post will be more likely to get attacked and commented on due to the nature of a post like this.
Note: On a personal level, I do acknowledge the practical utility of physicians because they do serve a very important function in all societies. They are healers and they are here to prevent and treat pathologies of the body. I personally think that for most people, our health is the most important aspect of our lives. When we are not healthy, almost nothing else matters. When we find out we have terminal pancreatic cancer or are badly mutilated from a horrific car accident, there is no question that physicians are absolutely critical in our well being and overall happiness. One of my cousins just finished medical school and is about to become a doctor and I have the highest respect for his intelligence, work ethic, and competence. Some of the most intelligent people I have ever met went to medical school at the age of 19 or 20 after skipping grades and high school to go to university directly. I only have great respect for physicians so this is only to provide a small critique on most physicians ability in answering the more difficult questions related to the real research available currently in the world on height increase. Most doctors just are not that informed or knowledgeable on this subject because they were never taught the subject in school or in their training.
Disclaimer: All opinions expressed/made by me in this post is only my own personal thoughts. I am not affiliated with any organizations, groups, or say health insurance companies which might be trying to undermine or question the professional authority and skill of people in the medical community with their 2 decades of schooling and training.
We all know that this endeavor to try to figure out a way to make ourselves taller by either increasing the natural growth rate or restarting another growth spurt after physical maturity is something that is not talked about a lot. A lot of people might like and do desire to be taller but very few people are probably willing to put in the type of time, energy, and commitment that people like me and the other height increase researchers do to really see if there is a real scientifically validated solution.
I am going to try to show in this post why most doctors/physicians who get trained in traditional accredited medical schools (like Johns Hopkins, Stanford and Harvard) may not be as equipped in answering the questions on Auxology (the study of growth) as we think they can. One’s profession does not determine one’s expertise in a subject.
A person can be an engineer but also be a really bad engineer. One might come out of Harvard Medical School but also end up never doing much except work in a large medical insurance backed clinical corporation or start a small family private practice with routine checkups.
In today’s age of degrees, accreditations, and certifications, and almost all types of professions, the medical profession is one of the most strict in terms of who has the stamp of approval. Almost always the stamp of approval in showing that a person is “good” enough to give real professional medical advice is that they made it through 4 years of Medical School, no matter where the school is from, as long as it is accredited. I think this type of mentality is dangerous since people in most societies has so much respect and admiration for doctors in general.
I personal have never heard a person who is some type of physician have other people say bad things about them, except maybe on their personality, but never their intelligence. If you are a doctor, everyone else will think you are intelligent and worthy of authority that can never be questioned.
There is a well known joke among Pre-Meds and medical students which goes like “What do you call a medical student who graduated last in his/her class?” Answer: “A doctor”
Note: For me, most things that deal with prestige mean little but it still might be useful to look at Medical School Rankings just for the sake of checking. From the annual edition on the “best”, highest ranked Medical School programs in the USA from US NEWS & World Report, Education, Grad School, 2013 Best Medical Schools based on Research, NOT Primary .. we would find that the top medical programs in terms of university include,
- 1. Harvard
- 2. Johns Hopkins
- 3. University Of Pennsylvania (where Dr. Carl Brighton is based at)
- 4. Stanford University
- 5. University Of California, San Francisco
- 6. Washington University of St. Louis
- 9. Duke University
- 10. University Of Chicago
- 10. University Of Washington
- 13. University Of California, Los Angeles
- 19. Mount Sinai School Of Medicine
From a quick glance we can see where most educators and maybe also the general public thinks the best doctors/physicians should be coming out of, at least in terms of USA based schools. Maybe schools in say China, Germany, Japan, Switzerland, or Russia might produce even finer physicians but I would have no way of really judging those schools and the students that come out of those schools.
I will be focusing this post on looking at 3 of the 4 highest ranked medical school programs in the program. They would be Harvard, Stanford, and Johns Hopkins Medical School program.
Most medical school do not dedicate an entire block or quarter to studying just the skeletal system in enough detail. And in my personal opinion they shouldn’t. In terms of the more critical organ systems in the body, the skeletal is one of the less important ones. When you are talking about a person’s life, the greater focus is on the heart and circulatory system, and the brain and the nervous system. The bones and cartilage that make up the skeletal system is rather straight forward, with the 200+ adult bones in the body, and where each are located. Once you have the nomenclature and location of the bones down, you move on to more important subjects like virology and immunology. What I have found is that only a portion of people will go into the two main subjects we do research in, Immunology and Orthopaedics. Even further, we can say that the subset of physicians which can give any reasonable explanation about our growth process is even smaller, coming from orthopaedic surgeons which have studied the various growth disorders, or maybe pediatricians which focus on the growth of children and adolescents.
My point from this part is to say that the number of people who both are physicians and have extensive knowledge on the details and mechanisms of human growth will be very small. From my research on the internet, pediatricians when asked about growth plate closure and further growth only state the general currently accepted views which is probably repeated thousands of times over around the world when a teenager kid asks them whether they will still grow taller after seeing the X-rays showing full ossification. It could be that they turn out to be right and that there is nothing we can do but they only seem to believe in the generally accepted view right now.
First, let’s see what Stanford Medical School has for its program.
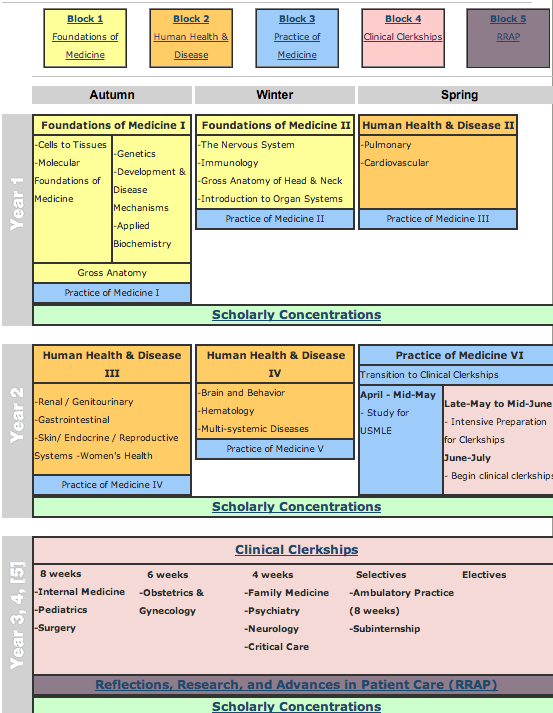 As we can see from the website from Stanford Medical School for the Overview of the MD Curriculum, one of the leading medical schools in the USA and the world, most medical school curriculum almost never focus much attention on the bones and cartilage of the musculo-skeletal system. Medical schools in general are almost always 4 years in length. Only the first two years in medical school is really dedicated to learning about the theory and mechanics of the body in any depth. The last two focus on doing rotations and shadowing physicians who are already practicing their specialities. Since a person is out in the field and not in the lab, they are learning the more practical skills needed to save lives, but the knowledge they learn will be from older, more experienced people.
As we can see from the website from Stanford Medical School for the Overview of the MD Curriculum, one of the leading medical schools in the USA and the world, most medical school curriculum almost never focus much attention on the bones and cartilage of the musculo-skeletal system. Medical schools in general are almost always 4 years in length. Only the first two years in medical school is really dedicated to learning about the theory and mechanics of the body in any depth. The last two focus on doing rotations and shadowing physicians who are already practicing their specialities. Since a person is out in the field and not in the lab, they are learning the more practical skills needed to save lives, but the knowledge they learn will be from older, more experienced people.
This means no real breakthroughs are made, unlike in research and the lab. So we have to see in detail what the curriculum does offer the medical student which might suggest that they would know enough to be conversationally competent in what we are trying to do and researching. In the years 3-5, the medical student does have a section for learning about pediatrics, which will teach them about growth and growth plates.
For the Stanford Medical School program above, it is broken up into 3 quarters, (or could be trimester thing) and there are 5 blocks. In each of the blocks, the students are expected to study like mad but you can see that only 5 quarters of the first two years is actually dedicated to reading and studying about the human body. It would seem that they zoom past the information about endocrinology which is lumped up with the reproductive system. There is obviously a type of introduction course on human anatomy and I would suspect that this is where they get any information about the bones.
If I was to take a guess, when any person has a skeletal injury like a fracture, they either go to the emergency room or the injury is not that serious that leads them to see a family doctor first. IN both cases, the bone injury results in the subject/patient ending up in seeing a specialist. This shows that for the majority of students coming out of medical school programs, they just don’t have that much experience looking at the subject of auxology.
Analysis And Interpretation:
If we look at the diagram of the curriculum and the details of the section of the diagram below we would see that no where does it seem in the curriculum do the medical students put a lot of their focus and study on the skeletal system.
For physicians, they have to pass 3 standardized tested known as United States Medical Licensing Examinations, the USMLEs. On a personal note, the reason why I might know a little more about the process to become a doctor than say the average person you might find on the street is because in my undergraduate years I considered for a short time taking the medical school approach, and spent a few days doing research on seeing what it would take to become an oncologist or hematologist.
Note #2: A substantial amount of my medical numbers and facts will be coming from a recently viral post made by Benjamin Brown M.D. on the topic of “The Deceptive Income Of Physicians” on his WordPress based blog HERE. As of the current time 1/28/2013 there is already almost 740 comments made on his really controversial and conversation stirring post. It is clear from me reading the comments that many of the other physicians who have read his post and numbers are questioning the validity of his numbers but I still think the values are reasonable and useful to be used in this post.
The details on the Stanford based curriculum is below.
Block 1: Foundations of Medicine
Autumn and Winter (Year One)
Autumn quarter consists of two components, with anatomy study throughout. The first component, molecular foundations of medicine and structure of cells and tissues (histology), builds a vital foundation for the scientifically trained physician of the future. The second component, exploration of molecular processes, continues with developmental biology, applied biochemistry and genetics, with open time in the schedule for students to explore scholarly concentration topics and/or elective coursework.
Winter quarter includes the immune system, the organization of the nervous system and the function of neurons, and anatomy of the head and neck. Principles of pharmacology and drug action and an introductory look at microbiology and infections of the respiratory system, provide the background for integrated organ system units to follow.
Clinical correlates in combined basic-clinical science sessions illustrate how basic science discovery translates into clinical practice.
Courses in the Foundations of Medicine block include:
|
Foundations of Medicine I
|
Foundations of Medicine II
|
| Applied Biochemistry (Bioc 200) | The Nervous System (NBio 206) |
| Cells to Tissues (Inde 216) | Immunology in Health & Disease (Imm 205) |
| Molecular Foundations of Medicine (Bioc 205) | Intro to Human Health & Disease (Inde 220) |
| Genetics (Gene 202) | Gross Anatomy of Head & Neck (Surg 203B) |
| Development & Disease Mechanisms (DBio 201) | |
| Gross Anatomy (Surg 203A) |
Block 2: Human Health & Disease
Spring (Year One), Autumn and Winter (Year Two)
Study units are organized by organ system and integrate histology, physiology, pathology, microbiology, and pharmacology. Organ system units cover normal structure and function, response to disease (including infection), and treatment (therapeutics). Morning sessions are correlated with problem-based cases and physical diagnosis skill training in the afternoon Practice of Medicine block. Final unit on multi-organ systems provides pathophysiologic integration of material from prior units.
The Faculty
Faculty members are chosen for their excellence and leadership in their respective clinical disciplines or fields of biomedical research. The Stanford medical school has more than 700 full-time faculty (two of whom are Nobel Laureates). We also have over one thousand adjunct clinical faculty who practice in the neighboring communities.
Organ Systems
The Human Health & Disease course approaches each organ system by block or thread, separated by quarter, as described below.
| Spring, Year One | Autumn, Year Two | Winter, Year Two |
| Pulmonary System | Renal System | Brain and Behavior |
| Cardiovascular System | Genitourinary System | Hematology & Hematopathology |
| Endocrine System | Multi-systemic Diseases | |
| Reproductive System/ Women’s Health |
Block 3: Practice of Medicine
Throughout Year One and Year Two, afternoon session, two days per week
The Practice of Medicine runs concurrently with Blocks 1 and 2, with clinical correlations to morning sessions to reinforce basic science concepts. Diverse teaching formats include large group lectures with team learning activities, small group (8-12 learners) discussions, smaller groups (2-3 learners) for clinical skills instruction, and one-on-one instruction. Variety of instructional methods include clinical problem-based cases, multistation exercises, simulations with standardized patients, videotaping with instructor feedback, and computer-based instruction.
Topics are organized within seven threads:
- Communication: Interviewing, history taking, psychiatric interviewing, sexual history taking, alternative medicine issues, cultural competency.
- Physical Exam: Normal surface anatomy, normal adult and child examination, gynecologic examination, geriatric examination, clinical procedural skills.
- MD in Society: Health care system, public health, bioethics, advocacy, public policy, international medicine, end of life care, domestic violence, preventive medicine.
- Quantitative Medicine: Epidemiology, information management, biostatistics, evidence-based medicine (EBM), introduction to clinical investigation, critical appraisal, exposure to scholarly concentrations.
- Nutrition: Principles of nutrition science followed by clinical applications in a series of web-based modules.
- Medical Practice: Skills training, professionalism, exposure to specialists, clinical teams, hospital information systems, clerkship mechanics.
- Clinical Correlation: Multisystem problems, development of problem lists, differential diagnoses, integration of basic science concepts.
Block 4: Clinical Clerkships
Begins as early as May of Year Two
- Minimum of 15.5 required clinical months
- Flexible scheduling with opportunity for broad clinical experience and/or continuation of scholarly concentration project.
- Clinical correlations in clerkships provide review of basic sciences.
Block 5: Reflections, Research, and Advances in Patient Care (RRAP) – Offered throughout the later years of medical school, this block – currently under development – will bring back the newest advances in basic science and reemphasize basic science applications for physicians.
 Now let’s look at our 2nd school, the golden standard which so many other universities and medical schools in the world might try to emulate in terms of quality, prestige, and authority, Harvard (cue in Bittersweet Symphony by The Verge or Eine Kleine Nachtmusik: Allegro by Mozart). Harvard Medical School along with Johns Hopkins University School of Medicine and Stanford School of Medicine have almost always ranked among the top 3 Medical Schools of the USA for many years now, if not decades.
Now let’s look at our 2nd school, the golden standard which so many other universities and medical schools in the world might try to emulate in terms of quality, prestige, and authority, Harvard (cue in Bittersweet Symphony by The Verge or Eine Kleine Nachtmusik: Allegro by Mozart). Harvard Medical School along with Johns Hopkins University School of Medicine and Stanford School of Medicine have almost always ranked among the top 3 Medical Schools of the USA for many years now, if not decades.
I will be taking a section from the Harvard Medical School Course Catalog 2012-2013 website HERE.
Health, Science, & Technology (HST) Courses
HMS – Division of Medical Sciences Courses
There is two other sections, Core Clinical Clerkships and Elective Courses (Clinical and Non-Clinical Courses) but I will not be looking into them since clinical clerkships happen almost always at the 3-4 year range. Some schools like Johns Hopkins and fewer of the more innovative medical schools these days are starting to add clinical work even earlier into the curriculum for the students to be better prepared for their residencies.
Analysis & Interpretation:
The first link to the preclinical courses in the first year shows that first year med students take 12 classes, and only maybe half of those courses is actually real hard sciences course. From my skim of the page, it seems that only one course, “The Human Body” will have the student actually get any new information about the human growth process. The second link for 2nd year seems to have only two real hard science courses, both of which would give the student only a cursory view of human growth mechanics. The Harvard Curriculum seem to push the student into the Clinical Internship role much faster, focusing on trying to make them better doctors in practice. After that, the years 3-5 (or 3-4) focuses more on the students getting out into the field and getting more hands on.
This shows again that even in one of the world’s best medical schools, they devote almost no time in looking in detail into the human growth process.
Now let’s look at our 3rd school, the curriculum from Johns Hopkins University School Of Medicine website HERE. The webpage I linked to the left is only for the M.D. Program Admissions, not the M.D./Ph.D. Degree option, the M.D.-MPH Degree option, or the M.D./MBA Program option.
From the paragraph of the page the message shows that the direction at which medical students should be learning the science of medicine is “organs, tissues, cells, proteins, and DNA” which shows how we go from a macroscopic level of analysis and learning down further further to a smaller and smaller level of understanding of the human body’s function.
From the page on “What To Expect“…
“This novel curriculum rejects the notion that there is “normal” or “abnormal” in medicine. Rather, everyone is on a continuum. The curriculum takes a systems approach to understanding all levels of the human being – from genes, molecules, cells, and organs of the patient on one end, to the familial, community, societal, and environmental components at the other end. The GTS curriculum integrates all of these variables to help students understand why patients present the way they do”
On the page, there is 3 links to 3 PDFS which explain what a prospective student who applies for admission to the MD Degree program should expect from their 4 years there. It would be in Year 1, Year 2, and Year 3 & 4, respectively.
Analysis & Interpretation:
If one was really dedicated they would go to the links and see that for Johns Hopkins program, they seem to take the Harvard approach which is for the incoming medical students to focus and get into the field faster. Theory and classroom learning is decreased, but still expected, sort of like the med. school expects the student to focus on doing the book learning at home and just know what they are doing and their mentors are talking about when they are doing their rounds or rotations, which they should.
Conclusion & Implications:
The whole purpose of this post was to show in a reasonably convincing way that what we are doing ultimately in trying to find a way to minimal invasively find a way to increase our height and grow taller after physical maturity and epiphyseal growth plate closure and cartilage ossification (beyond just limb lengthening surgery) is not a completely worthless attempt that has absolutely no chance of success. Although maybe after 10-20 years of intensive research we may come to that conclusion and we as height increase researchers are proven wrong, I would hope to leave this website and project around as a legacy and the #1 authority on this subject on the internet. This website is also supposed to be used as the ultimate resource in doing reviews on any marketed products and scams out there.
Nearly all medical professionals if you asked them would say that what we are attempting to do is impossible. Most people would never question their family physician or a surgeon’s authoritative word. I am saying that even the students that come out of our “best”, most prestigious medical schools don’t really know as much about this subject as we do, so most of them should not be people we turn to for authority on answer our most basic question, “Can we still grow?”. They would say no.
What I am trying to do i to show that from many medical professional’s own schooling and training in their weakness and holes in knowledge, they don’t really have the full picture and done as much research on the subject of potential (not absolutely guaranteed) height increase. However that does not means that they can’t easily catch up to our level of understanding and research and be just as knowledgeable as us on the subject. They could very easily.
One of the things that even physicians who have finished their residency and fellowships still have to do is keep up with the recent medical breakthroughs and developments by reading medical and research journals. Physicians are expected to renew their medical license every few years so make sure they still have that high level of competence.
They know a lot, but if we want to make the real breakthroughs, we have to know about our area of study better than any physicians to be able to prove them wrong, in the eyes of objectivity and hard science.
On a related note, I would like to say that I have gotten emails from people who are either currently in medical school right now or doing their residency (1st or 2nd year) and they say that they have been personally following Tyler’s HeightQuest.com blog for years and this blog/website recently because what we write in our content is stuff that they are never exposed to in their medical schooling curriculum, or in their residency programs.

Pingback: AA vs. Doctors
Pingback: Padlet Strategies from Education 540 – Site Title