This seems like a reasonable question to ask when a person who is past bone maturity and physeal ossification is interested in learning how they can grow taller.
Well, to answer this question, there are many factors and variables we have to take into consideration. It is really hard to give a definite answer, although I have stated before that we might be as close as 15 years away from some commercial company developing the technology to do that. On the other end, it could be as far away as 50-70 years, assuming that the rate of progress continues for the fields of tissue engineering, regenerative medicine, 3D Bio-printing, and stem cell R&D. Let’s remember that the rate of scientific/technological progress for the biological sciences and biomedical application does not follow the trajectory of Moore’s Law, unlike electronics and Computer Science. To make progress and breakthroughs in BIology is extremely resource/financially intensive, unlike CS, which often just requires a programming wunderkid sitting in his underwear in his dorm room eating Cheetos.
I revealed in a post a month ago about the company EpiBone who is developing osteochondral grafts as implants which has as an advisor Dr. Warren Grayson, who I have said since 2013 is one of maybe 6-7 researchers in the world we should be following. Refer to the post “EpiBone Company To Engineer Osteochondral Grafts – Research Breakthrough!“. The company reveals that there are definitely plenty of people who realizes that there is a huge financial incentive to get this technological problem to work out. There has already been at least 1 patent filed by the research group at EpiBone on how to use a bioreactor to build bone tissue. Refer to “Methods, Devices and Systems for Bone Tissue Engineering Using a Bioreactor – US20120035742 A1”
Let’s now look at the research of Dr. Robert Tracy Ballock, who I have said is the other main researcher we should be following. His work has been on the Growth Plate for the last 15 years or so. He has been working with Dr. Eben Alsberg, who showed that it was possible to growth a functional growth plate. Refer to his grant on Growth Plate Regeneration available here. Further searching on this grant and his work shows that there was 2 grants, one for the 2012-2013 period, and a 2nd grant for the 2013-2014 time frame. (2012-04-11 – 2014-09-30). If you search around the internet for any new academic papers published under Dr. Ballock’s name, he has not published anything for this year, or even late 2014. I would guess that he is finished with his research from the grant which lasted 2 years and plans to write something up. There might even be a Patent application that is filed from his research soon. Whatever he has found, he is not revealing it yet, at least not to the general public.
3 months ago there was a biomedical conference where a university researcher named Dr. Juan Taboas (Ph. D) presented his work called “Repair and Regeneration of the Physis” at the Houston Methodist Research Institute. Just two months ago, the video of his presentation was available for the general public to watch, but now that video has been set to private and one requires a password to watch the video. I did watch maybe the first 5 minutes of the presentation, which was over 1 hour long. There was a video/audio syncing problem so I was not able to record the presentation back then. The part I watched was not that informative and did not reveal too much about his current research.
The abstract of his talk is below…
Physeal regeneration poses a considerable challenge in orthopaedic regenerative medicine. The physis is the cartilaginous interfacial structure at the ends of the long bones that produces appendicular skeleton growth. Fracture, infection, and cancer can result in limb deformity and loss with significant morbidity and medical cost despite their status as rare disorders. Dr. Taboas and his research group are developing hydrogel and stem cell based point-of-care therapies to prevent and repair limb growth disruption in pediatric patients, and for endochondral repair of large boney defects in children and adults. They are currently evaluating the effect of hydrogel composition and zonal patterning on construct growth and architecture maintenance in an in vivo murine subcutaneous implantation model. These techniques may be applied to regenerate other skeletal tissues that require appropriate interfaces with bone for proper function, such as articular cartilage and ligament.
Here is something that the average reader needs to understand. There is a branch (or maybe sub-branch) in the medical research fields known as Orthopaedic Research. Technically, orthopaedic research refers to diseases and injuries of bones, joints, nerves, and muscles. However, there what is not written, but also implied is the cartilage and the tendons as well. Keep this note in mind as we go further along.
When I was at the 2nd Organ-On-A-Chip and 3D Bioprinting Conference in Boston a month ago, there was a presenter at the conference who revealed that she and her group was working on getting stem cells to build tendon tissue. Tendon tissue is what connects muscle tissue to bone tissue. It is similar to cartilage, because of the high level of collagen, although not the same type of collagen. Her presentation was ” Engineering Tissue Microenvironment Informed by Development, Healing and Disease”. Refer to Catherine Kuo, Assistant Professor at Tufts University. Apparently, she got her postdoctoral training in the Cartilage Biology and Orthopaedics Branch at the NIAMS of the NIH. The last I heard, she was changing positions to a different university. This shows that the field of stem cell technology is being applied to form every type of tissue.
There was a paper that was being passed around at the conference which asked all the people at the conference what type of tissue they planned to use the 3D Bioprinter on. The type of tissue that was most often formed from the 3D Printers was cartilage. Not bone, not vascular tissue (blood vessels like capillaries), not tendons, but cartilage. This reveals something critical. It seems that all of the major researchers understand what would be the easiest type of tissue one can print using this new form of technology. Everyone is thinking the same thing, and we are almost all pursueing the same idea: Cartilage.
I would guess that a large percentage of the research done in this well known field known as orthopaedics is on cartilage research, specifically cartilage growth and regeneration.
So what does Dr. Grayson, and Taboas have in common?
It turns out that they both were all at the 2011 Termis Regenerative Medicine Conference in Houston. Their names was on the list of Attendees. I was supposed to go to the 2015 Termis Conference in Boston, but the cost was just too high for me. Dr. Atala of Wake Forest was going to be there. If you plan to take this type of research seriously, you have to spend the money (about $2,000) to attend these types of exclusive conferences to learn what the real academic researchers are working on.
What about Dr. Ballock?
He is a medical doctor as well as a researcher since he has both a Ph. D.and M.D. (Smart guy). Like all academic researchers, he is involved in a lot of societies and academic groups. I am sure he flies around a lot to give presentations and talks in various conferences and conventions. Back in 1998 he was at this conference called “Bioengineering & Orthopedic Science – Gordon Research Conference” which is now known as “Musculoskeletal Biology & Bioengineering”. It was held from July 26-31 in Andover, New Hampshire. He gave a talk called “”Control of Cell Proliferation in the Growth Plate”. It seems that for almost 2 decades this guy has been working on getting the growth plate to work out. He was involved in this multidisciplinary conference back in 2008 called the “Cleveland Clinic Cartilage Innovation Summit”. The conference was basically a group of researchers gathering to talk about the subject of “The Clinical Science and Outcomes of Cartilage Repair, Maintenance, Regeneration and Replacement”.
So What Am I Trying To Conclude From All This Information?
Some people who are in industry who focus mainly on earning income and profit for their employers and no longer in academics (who focus mainly on the research, discovery, and learning more) would say that something along the lines that all the breakthrough research discoveries one finds in the university lab is still useless if one chooses not to bring their findings into real application and shared with the rest of the world.
This applies to the field of Orthopedics (and most any other type of medical research). What I have found in the last 6 months from attending the conferences which talk about the rising field of 3D Printing, and specifically 3D Printing applied to tissue formation is that the researchers in the university labs are trying their hardest to bring their research to the public.
Dr. Grayson is going to help EpiBone succeed in getting bone implants to work. There is already too many companies who have gotten the theory and science down on getting lab grown stem cell derived bone tissue to be reimplanted into the subjects body with complete success. The 1st step in getting bone tissue to be grown from stem cells or mesenchymal stem cells has been multiple times with the academic researchers forming companies to get their research out to possibly make them millionaires. There is no problem with this since the academics see a way to make personal gain from their years of hard work and research.
When we then move towards the 2nd/next step of getting fibrocartilage to be printed from lab grown pieces of cartilage or chondrocyte, there are labs like Dr. Atala or Dr. Lawrence Bonassar who have already achieved that too. You have seen many pictures of the outer ear lobe being grown in the labs in cultures and even on the backs of lab mice. The same can be said about nose tips, which are also fibrocartilage.
The 3rd step is to get Hyaline Cartilage to be printed or grown in the lab. We are getting super close to getting Hyaline cartilage to be printed. There were 2 exhibitors at the Organ-On-A-Chip Conference, (Cellink and RoosterBio) who would be able to provide the raw materials, cell culture medium and seed mesenchymal stem cells, to let any professional lab to play around to eventually get the lamellar structure of hyaline structure to work out. I would be willing to guess that by the time the 2020 Termis World Conference comes around, we would have succeeded there.
Should we try to the traditional seed stem cell into scaffold method or should we try the more revolutionary way of growing cartilage tissue from scratch using the 3D Bioprinter? – We would have to make that decision eventually.
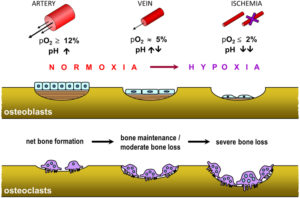
The 4th step would be to get Epiphyseal Hyaline Cartilage to be grown/printed. Ballock has been working on this problem for 20 years. He got a grant for the 2012-2014 time frame to go research on growth plate regeneration. It is not just him who is working on getting this thing to work out. In the grant, he wrote that if he is successful, the growth plate regeneration technology can be used by people who have already reached bone maturity. He knows what his research would mean and how it would effect the public.
Of course, orthopaedic research and development is something that thousands of people around the world are working on. He is not the only one trying to get growth plate regeneration to work out.
- There has been teams in Hong Kong who got the chondrocyte implantation idea to work back in the early 2000s. Based on certain Non-Disclosure Agreements (NDAs) I signed early on, I can not reveal the exact details of those studies, only to say that the experiments were done and were successful.
- I revealed early on, in the late 2012 that there were military hospitals in China who have gotten growth plate transplantations to be successful. Where did they get the growth plate in the first place is still suspicious though.
- I wrote about the fact that even plastic surgeons in Russia, like Dr. Teplyashin have gotten the scaffold technique to be successful but this controversial technique is probably only offered to Russian millionaires in secret for maybe $200 K a pop. They got it to work out in sheep, but that doesn’t mean they have ever performed the same surgery on humans.
The truth is that we are getting quite close, with the best option being people like Ballock. If he is willing to write up his results from his work for the last 3 years, and take those results and form a company around it to develop growth plates grown out of scratch (ie 3D Printed) or based on the traditional tissue engineering method using scaffolds and growth factors, he would have something working in 10-15 years. Of course I could be way too optimistic.
To answer the original question, I would make a very tentative guess based on the idea of Kurzweil’s Law of Exponential Growth, if someone like Ballock is willing to form a company around his discoveries and try to bring it to public, we would have a limb lengthening alternative based on 3D Bioprinting, Stem Cells and Scaffolds, and tissue Engineering within 10-15 years with enough funding. When it comes to funding, I would say that biomedical engineers and researchers would need maybe at least $100-$300 Mil to get this procedure out to public. So who is willing to fund this type of project?