Updates For Regenerative Tissue Engineering Using Stem Cell For New Growth Plates – How Much Longer?
So the most recent relevant post I had written had said that we would need to wait 30 or even 50 years before the limb lengthening surgery alternative would be finally be available. That made many people very upset that this idea which I had claimed to be “almost there” would still take that long. Let me try to give you guys a better estimate on what is reasonable to expect to happen within the 21st century in terms of biotech.
The short answer is this. If we were to be extremely optimistic, It would take 10 years for the stem cell technique to be viable for for humans to use, but only for real medical issues. Within 5 years, the physicians performing the technique would realize that there is a large financial incentive in using the stem cell approach on people for cosmetic reasons. So being very optimistic, it would take 15 years before we can finally have the chance to use the new growth plate method. On the opposite end, it would take maybe 30 years for the stem cells to have all the technical details worked out for them to be for use for humans, and still another 10 years before doctors are willing to put the technique for use to lengthen bones. So the worst we can do is wait 40 years. Yes, it sucks that it could take almost half a century, and maybe some of us might not even live that long, but biological science is not like computer science, where you have dedicated people who can pump out a new product in a dorm room with a computer working 24 hours a day.
Here is something else which we need to consider. Exponential Growth. When we remember Ray Kurzweil’s Law of Exponential Growth/Returns which is supposed to signal the point known as the Technological Singularity, it suggest that maybe, just maybe the technology may come even faster, if the exponential growth of technological advancement is true. That might mean that at the earliest, the idea of implanting new lab grown growth plates into bones to lengthen the bone might be available for at least young kids suffering real orthopedic limb angular deformities within as close as 5 years, and have it available for adults for cosmetic application within 10 years.
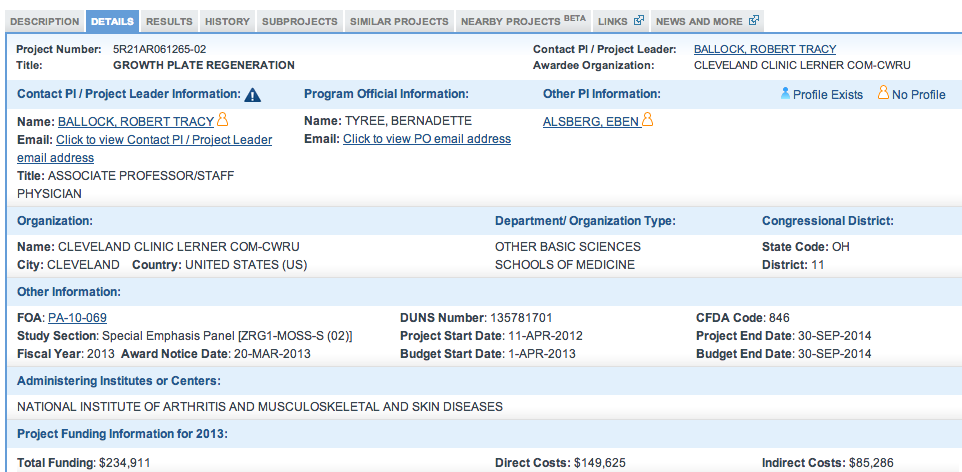
Let’s give you guys some perspective. If you guys typed into Google right now the term “new growth plate”, you would find as the first link a article/reference to Dr. Robert Ballock’s research at the Cleveland Medical Clinic. That shows that Ballock is very serious on getting the technical details on lab grown growth plates to work out. His desire is to use his knowledge from Harvard to help young children to correct bone grown irregularities. The article you find #1 in Google Search is called “Regrowing Growth Plates: A Fix for Kids’ Injuries? Promising research to mend growth-stifling plate damage” was written back in Feb of this year, 2014. The website by Cleveland Clinic showed that he is focused on the research, and his grant (which we linked to on the previous post) revealed that the project would end around August-Sept this year.
Quote… “In test tube studies, Dr. Ballock’s research team developed a 3-D cell culture model that replicates the key features of what appears to cause growth plate cartilage to develop in the column-like shape that leads to lengthening of the long bones in children.”
At the end, Ballock stated in typical research fashion that his research would be years away from being used for real application. This is disheartening to many teenagers and young people who want to be taller NOW and want something as soon as possible, but it takes time. Even when you want to use the stem cell approach for cosmetic use, other entities can resist you and your research.
The recent reveal that Alexander Teplyashin’s team in Mocow, Russia in getting bones to lengthen by implanting culture grown “growth plates” and trying them out on ram/sheep shows that in theory and concept, the stuff would work. However, Teplyashin is still a researcher (actually has a Ph. D in plastic surgery) and he must follow the guidelines and protocols that the academic and corporate rules set for him.
Here are some problems that have caused the whole stem cell research to be resisted. When George Bush was president (the 2nd one) he imposed laws which made it not possible for USA based researchers to use embryo derived stem cells. Because of Bush, the research into stem cells was halted for his entire 2 terms, which was basically a full decade. While the USA was held back, other countries in the world like Japan, South Korea, Germany, and Russia rushed forward and was willing to take the chance the Americans were not. It wasn’t until 2009, when Obama came to office did the law against stem cell research (at least the embryo derived ones) get lifted. (source: Obama Lifts Bush’s Strict Limits on Stem Cell Research).
The 2nd problem is that Teplyashin’s research has also been halted by the government branched in Russia, one source we found stated. His team is written up grants, petitions, and proposals to move forward in their research, but the government seems to be blocking his team from further progress.
All of this may sound like really bad news, but there is a LOT of good news which I have found recently which shows that the endeavor is definitely being pushed forward.
The Good News
Good News #1 – On the problem on cartilage material strength and whether it can handle the upper weight loading – It seems that this is not a problem. I do read a lot of reddit threads and on one reddit thread, where people were talking about the possibility of getting lab grown cartilage transplanted into their knees for pain management and osteoarthritis treatment ( http://www.reddit.com/r/science/comments/24gghv/for_the_very_first_time_engineers_have_grown/) it was revealed that cartilage that is created in the lab synthetically can withstand the weight load, with the high enough equilibrium compressive strength/modulus. Refer to the study Comparison of the equilibrium response of articular cartilage in unconfined compression, confined compression and indentation for more information.
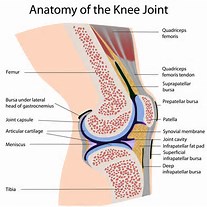
Good News #2: The problem that the people who want to fix their knee articular cartilage degeneration have cleared up is that cartilage implants like autologous chondrocyte implantation has not worked too well to the defects on the surface of articular cartilage. The problem is that the neo-cartilage tissue doesn’t seem to be able to fused properly with the older, natural cartilage. The cartilage then turns into the fibrocartilage tissue type. Of course, these guys on the Reddit Science Thread wants to add cartilage to an area of the body where there is already cartilage. As we know, cartilage is an anareobic environment aka avascular, where the cells inside the ECM of the cartilage can’t get nutrients through blood vessels. Of course then it would make sense that plopping new cartilage on top would not work out too well, since traditionally you need vascularization to get the transplants to fuse with the rest of the body. Our desire is instead to add cartilage to a place where there is no more cartilage (fully fused) and only bone. Bones are very nicely vascularized. In fact, we reported news recently that the vascularization issue was figured out by Teplyashin’s team in a paper that they published (How Svetlana Zagirovna Sharifullina Developed A Vascularized Fully Functioning Growth Plate)
(Side Note: Here are some places which I regularly read up on and make sure I keep up with the most up to date information on reconstructive tissue engineering, stem cells, and such. http://www.reddit.com/r/science, http://www.reddit.com/r/stemcells, http://www.reddit.com/r/tissueengineering, http://www.reddit.com/r/Futurology/, http://www.reddit.com/r/orthopaedics, http://www.reddit.com/r/cancer . In addition, I also read up on the works for the dozens of researchers cited http://www.beckersspine.com/spine/item/14329-10-spine-surgeons-researching-disc-regeneration)
Conclusion:
So when it comes to the technical problems of getting the synthetic lab grown growth plates to meld with the surrounding bones, which is usually just a vascularization problem as Hakkers stated in our interview years ago, that seems to have been resolved.
And when you look at how strong the lab grown cartilage really are, looking at the values of the equilibirum compressive modulus, you find that the major issues that I have come up with seems to be almost all gone.
The few problem that I can think of is that the scaffold derived epiphyseal hyaline cartilage is not producing enough ECM organic compounds, most specifically Collagen Type II, the GAGs, and proteoglycan. However, I would suspect that the technical issue would be a rather easy one to figure out. The other thing is how would the surgeon make the right type of cut into the epiphysis-metaphyseal connected region to implant the cartilage. If you look at how real cartilage is layered in the human body (I saw off the end of a dead young pig’s leg), they are not flat, but curved and bumpy, which is probably due to the different rates of chondrocyte columnar activity.
Then when you look at how easily it is for people with a 3-D printer to print out layers of hydrogel and scaffolds these days, with maybe dozens of people doing similar research, things seem to be looking very good.
I don’t want to make it sound too positive, since there will always be huge issues. The article I found written by someone at Regenexx over the fact that Mesoblast spent hundreds of millions but still couldn’t get their human subjects to have similar results as their lab rats show that sometimes the best results on lab animals can not be translated to humans. The article back in May of 2013 MAJOR STUDY UPDATE: STEM CELLS EASE BACK PAIN revealed that while the subjects did indeed decrease back pain, the disc height did not increase like what happened in the lab with the rats.
Harald Oberlander who I have been in contact with referenced Mesoblast’s research to the people on the Make Me Taller forums but I don’t think even he is aware of the most up to date releases that is coming out of the company. Progress is not easy.