So I stalled out in the old method at 75 1/4” for a long time(several months), it wasn’t until I tried this method that I started increasing the measurement again. I also increased the duration and am moving the vibration device around the hand more. That could play a role.
The old method took me from about 75 to 75 1/4”. I don’t know why I stalled out. Could be over time the body adapts to this stimulus and with this method I too will need to add other modalities to make it more effective.
Here’s the video demo:


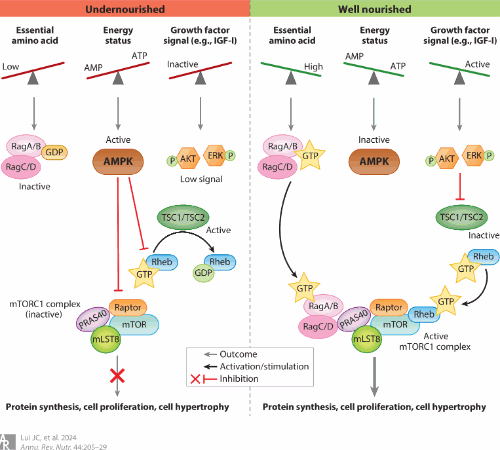
Essentially what I do is I grip some oddly shaped objects for torsional loading. The more oddly shaped and weird the objects the better. You could also use bands, etc. ideally you’d the want the bone to have as many areas of compression and tension as possible. Fluid flows from areas of compression to areas of tension so the more areas of compression and tension there are there. The more fluid is going to flow.
Vibration is another stimulus to enhance fluid flow. The closer the vibration is the target bone/cartilage the better.
As seen in the video I kind of stir the hammers as a way to get more torsional loading and activity in the muscles. Muscles pull on the bone via the tendons creating more elastic bone deformation
The reason for changing the bones axis in relation to gravity I explain below in a an email to Hiroki Yokota the pioneer of the Joint Loading Modality and an expert in fluid flow to stimulate anabolic responses in the bone:
“You mention that the reason why lateral loads in bone is so effective is because of the water bottle analogy in pressing to the side is more effective in moving fluid.
But inversion/eversion is even more effective in moving fluid in the water bottle analogy and the arms undergo rapid eversion/inversion much more frequently than the legs.”
Hiroki Yokota’s response : “
I think your idea may work but we need to think about a basic fluid motion. A Navier-Stokes equation has three major forces to alter the flow. They are:
- Pressure change
- viscosity
- gravity
Since viscosity is to prevent the flow, two driving forces to generate flow are pressure change and gravity. Lateral loading induces pressure change, while inversion activates gravity. We need to evaluate quantitatively the effects of loading-driven pressure change and inversion-induced gravity on fluid low in a bone matrix.”
Below are some studies that show that gravity can alter fluid flow in the bone and can stimulate cellular activity:
http://www.heightquest.com/2011/04/get-taller-stature-with-inversion.html?m=1
According to Fifteen days of microgravity causes growth in calvaria of mice. , microgravity alters interstitial fluid flow. Inversion and eversion would mimic this.
The Effect of the Microgravity Rotating Culture System on the Chondrogenic Differentiation of Bone Marrow Mesenchymal Stem Cells., microgravity rotating culture increased the chondrogenic differentistion of mesenchymal stem cells. Inversion and eversion would mimic this.
http://www.heightquest.com/2011/04/space-and-height.html?m=1
That interstitial fluid flow can stimulate bone response is not controversial. That this response includes making the bones longer is controversial. However, baseball pitching, tennis, and arm wrestling all of which have anecdotal reports of increase in bone length all have changing the bones axis in relation to gravity. Diving is the closest thing for legs that I could find that increases bone length and it also has constant rotation inversion/eversion to change the bone’s axis in relation to gravity.
I believe that interstitial fluid flow can make bones longer if this stimulus is sufficient. The reason that arm bones are easier to grow than legs is because the hands can grip things so the arm bones get more direct loading.
Think of an hourglass:
You tip it over the sand moves from one to another but not all right away(the rate at which it flows is affected by vicosity). You could affect the rate by which the sand flows by compressing the sides of the hourglass or vibrating the hourglass to make the sands move faster.
Interstitial fluid flow has the ability to affect osteoblasts, osteoclasts, and stem cells all of which could potentially combine to make a bone longer. The exact mechanism of how this could happen is not yet known. But if interstitial fluid flow can affect all these cells and can affect gene expression then it suggest that there is potentially a method by which interstitial fluid flow can increase bone length is possible even if the exact mechanism is unknown.
The arms are subjected to much better loads than the legs are. Legs are not typically inverted. They femur is kind of inverted in a squat or deadlift but the weight is not close to the femur it’s on the back or in the hands. Standing hamstring curls are typically done on machines which are not as an effective a loading as actually gripping the weight and it’s hard to grip weight with the toes. Iron boots perhaps? Kicks are typically not loaded. I am trying leg swings with ankle weights but the ankle weights are only 20lbs more weight may be needed. reverse crunches also involve inversion of the legs but weight/torsion needs to be on the leg itself
Torso is typically only inverted in good mornings and decline sit-ups and cartilage is easier to stimulate than bone since it is a softer more easily deformable tissue but the issue is it has a poor blood supply so it grows slower.
Finding ways to apply this method if it works can be done for torso and the legs but it will be more challenging.
One other person has reported growth with this method but he was under 25 but over 18 so it may have been natural growth since arms grow longer for longer.
I was originally going to shoot for x-rays around 75 1/4” but that was before I stalled out originally. I want to see a rate of consistent and steady growth. I do have before x-rays. I want some experimenters to try and validate the method. I also think 1/4” is not strong enough above measurement error.
Most people want to move on to the legs already but the legs are harder it needs to be validated on arms first. Wingspan was chosen because it’s easy to see when wingspan begins and ends and I do get some variance in measurement but I go for the peak measurement.
So next phase is:
Try to gain more in wingspan at a steady rate and validate with X-rays
Try to get experimenters to validate. I have gained wrist thickness and muscle mass with this so it has other benefits too. Other experimenters will reduce personal bias.