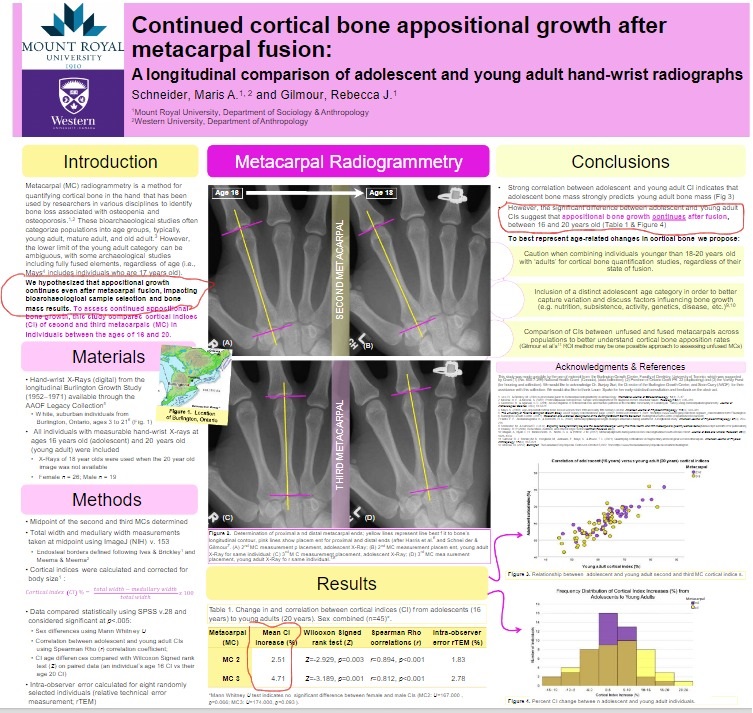
There is a lot of evidence that shows that bite jumping appliances and other dynamic loading methods can induce growth of the jaw. This growth seems to be due to the lateral pterygoid muscle applying dynamic load on the mandibular condylar cartilage. There, is a possibility of applying these same techniques to other long bones. Other bones however do not have this muscle insertion so directly into the cartilage. We would have to think hard to find a way to apply this technique.
Long-Term Effect of Diet Consistency on Mandibular Growth within Three Generations: A Longitudinal Cephalometric Study in Rats
<-harder foods likely work by forcing the lateral pterygoid muscle to work harder in a more dynamic way thus placing a stronger load on the mandibular condylar cartilage. One thing that would be interesting to try is if this worked on adults.
“Craniofacial growth has been shown to be affected by different factors, including environment. It is thought that environmental changes could possibly affect the growth of the mandible. The question of how diet consistency affects mandibular growth within one generation of rats has been answered to some extent by various studies, according to which diet consistency may result in different masticatory forces that affect mandibular growth. There is no study so far that examined possible quantitative and qualitative growth changes in the mandible within different generations. The present experiment evaluated the impact of different food consistencies on mandibular growth within three generations. The results of this study indicate that a soft diet could be responsible for less mandibular growth, and this information might be passing through generations.”
“A total breeding sample of 60 female and 8 male Wistar rats were used in this study. Measurements took place only on female animals. Twenty female Wistar rats at 30 days old and four male rats at 30 days old comprised the primary breeding sample of the first generation, and from these animals two different generations were reproduced. Lateral cephalometric X-rays were taken from all female rats at the age of 100 days.”
“Means of measurements of all soft diet groups compared to hard diet groups were significantly smaller. According to linear measurements, there was a significant difference only between the first-generation soft diet with the third-generation soft diet group. According to geometric morphometric analysis, the statistical differences appeared on the condylar process and the angle of the mandible”
“muscular loading forces play their own part in bone growth and development. One of the most critical muscular systems is the orofacial, which is necessary for feeding in vertebrates. Mandibular growth is closely associated with the movement of the jaws and loads of the orofacial region. Mastication, as one of the environmental factors, seems to be responsible for a variety of developmental changes in the craniofacial region and more specifically in the mandible”
“The coordinated actions of osteoclasts and osteoblasts result in the resorption and replacement of the existing cortical bone, a process known as intracortical bone remodeling (or simply remodeling). Secondary osteons, which are cylinder-shaped structures, are created as a result of this process. Due to their concentric lamellae and surrounding cement line, secondary osteons are apparent in cross-section. The remodeling process’ resorption phase releases mineral reserves to support mineral homeostasis, but it also leads to the development of microcracks as a result of mechanical deformation. Both significant mechanical deformations (high strain) and repeated cycles of loading have been linked to microcracks. Therefore, areas of the skeleton with more severe loading conditions should have increased rates of remodeling since those areas should sustain more microdamage. When the load situation is unknown, it is less evident if increased remodeling may be attributable to high strain or cyclical loading.” <-they suggest that the loading may cause microcracks and that could cause the change in bone shape but I think the increase in size is due to articular cartilage endochondral ossification.
“high strain may not be necessary for substantial remodeling to occur and that cyclical loading may be more likely to result in elevated remodeling”<-this alludes to fluid flow theory.
“various epigenetic mechanisms are now known that consist of intracellular macromolecular chain reactions and extend from the membrane to the cell nucleus. In this way, information is transferred between the extracellular environment and the nucleus. The osteocyte network detects and responds to mechanical stimuli and thus plays an important role in triggering bone remodeling. In addition, loading applied to the tissues can change the shape of the cells. As a result, deformation of the intracellular content, including the cytoskeleton, is observed, and processes are activated that even change the mechanisms of action of the genome”
“Increased mineralization was found on the trabecular bone in the condyle of the hard diet group than in the soft diet group”
“chewing hard food enhances nearly all physiological masticatory parameters, muscular coordination, and masticatory side modifications as compared to chewing soft food”<-the question becomes whether we can keep chewing harder food to gain more in the mandible.
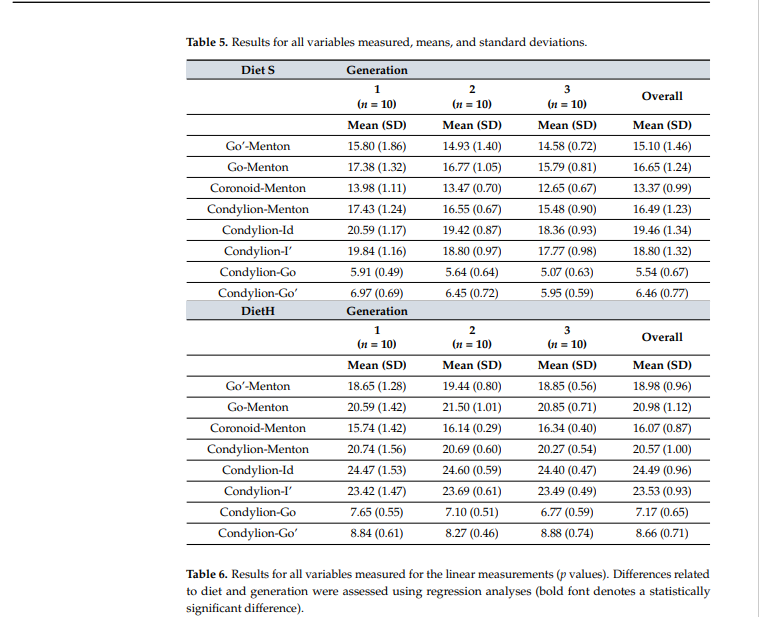
Every dimension was superior in the harder food group.
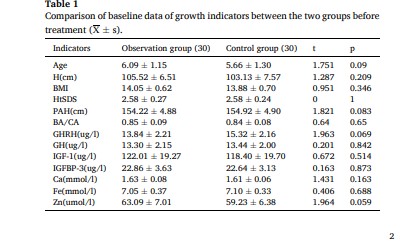
“The indications for the posterior mandibular height were Co-Go, Co-Go’ linear measurements. There were statistically significant differences between all soft diet groups when they were compared with the hard diet groups in all linear measurements. There were no statistically significant differences between all hard diet generations due to linear measurements.”
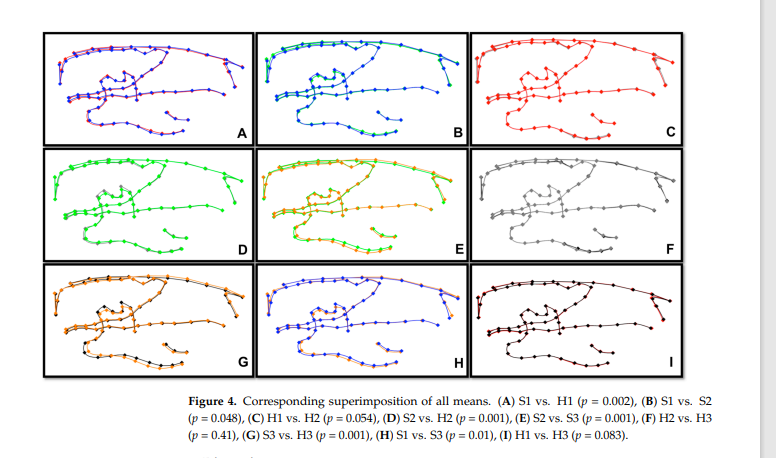
Definitely noticable difference in the G group.
“In 2014, Hichijo et al. found that there was no significant difference between the hard diet and soft diet groups in the mandibular length and the mandibular base length”
“It is important to mention that we used a similar methodology to previous studies, but with some of these studies, our results differ in terms of one-generation outcome. This could be possibly explained because we used a different rat strain than some of the previous studies. Another possible reason could be the limitations of 2D X-rays and the procedure that each study followed to take those.”
So this study provides further evidence that mechanical loading can influence growth of the mandible and we can possibly apply those principles to alter the growth of other long bones.