Using Autologous Mesenchymal Stem Cells To Treat Hip and Knee Joint Pain from Osteoarthritis
I stated about 2 months ago that I wanted to expand the scope of the research that is done on this website, to include other subjects like the biochemistry of cancer, orthopaedic conditions, and similar issues. These next few posts will be dealing with this subjects. Some of the information will be related to what I’ve been researching before.
There was a very recent article (came out on August 3, 2014) that came out in the Australian news website The Age entitled “Stem cell trial hope for osteoarthritis sufferers” which showed that MSCs are being used to treat people who are suffering from knee pain associated with Osteoarthritis. While it may not seem too revolutionary and profoundly new to us who are so used to reading up on Patents and University backed cutting edge research on stem cells, this method would still be very interesting to a large group of the population who are suffering from joint pain from cartilage degeneration.
As the article says, a middle aged female underwent liposuction so that her fat can be sucked and then filtered to get the little bit of stem cells in her fat tissue. Those stem cells will be then be packed together in pure stem cell and high density form, which are injected into her hip joint region to relieve pain.
When looking at the overall procedure from a higher level, I am reminded of a similar type of procedure that is being done by Dr. Peter Wehling at Dusseldorf which is now called the Regenokine/Orthokine method as well as the Platelet Rich Plasma therapy. In all of these methods, the entire thing is minimally invasive.
The hope for the researchers who took the women’s fat out is to get the filtered stem cells to slow down the rate of cartilage degeneration in the woman’s hip. If that is possible, then the need for the complicated and expensive hip prosthetic replacement surgery can be pushed back by more than a full decade. The primary researcher is a Dr Julien Freitag, who would reference a South Korean study. I took the time to track down that exact article and found it. It is suggested in that Korean study that instead of just a single injection of the person’s own adipose derived stem cells, multiple injections will have much better results.
There will also be a 2nd study looking at how this autologous MSC method would work for cartilage lesions which are the result of trauma which often lead to the onset of osteoarthritis after maybe just 4-10 years after trauma.
The name of the article that is referenced is “Infrapatellar fat pad-derived mesenchymal stem cell therapy for knee osteoarthritis” which is associated with the Department of Orthopedic Surgery, Yonsei Sarang Hospital, Seoul, South Korea. The same group of authors had written also the paper “Mesenchymal stem cell injections improve symptoms of knee osteoarthritis.” which was published in April of 2013.
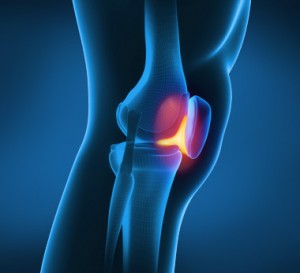 In the referenced article, the researchers took the stem cells from the infrapatellar fat pad region (aka Hoffa’s Fat Pad). Refer to the picture to the right for reference to where the fat pad is.
In the referenced article, the researchers took the stem cells from the infrapatellar fat pad region (aka Hoffa’s Fat Pad). Refer to the picture to the right for reference to where the fat pad is.
The stem cells which are isolated are then injected percutaneously into knees that have been suffering from arthritis.
Note: I might have made a mistake on assumption before. It seems that the method of PRP is used in this technique. Quoted from the article…
“After the stem cells were isolated, a mean of 1.89×106 (range, 1.2–2.3 × 106) stem cells were prepared with approximately 3.0 mL of platelet-rich plasma (PRP) and injected in the selected knees of patients in the study group. ”
I made the mistake of assuming that the stem cells would be reinjected in the body percutaneously and intraarticularly by themselves. I forgot to realize that the platelet-rich plasma would be used as the semi-liquid transport medium since stem cells by themselves with no medium would just shrivel up and dry out. This method is a type of PRP therapy.
After the first injection with stem cells and PRP, 3 mL of PRP was administered every 7 days as the second and third rounds of treatment. The results from the control group and the actual tested group were statistically significant.
Implications
From my search throughout the hundreds of patents for application of stem cells, I’ve already seen at least 2 groups which have put a patent on the technique on using MSCs to treat osteoarthritis or arthritis in some way, whether by the PRP method or some other idea. I quote was is said in the paper “With regard to in vivo studies, the transplantation of MSCs into full thickness articular cartilage defects has been attempted under various conditions.” so there has been many attempts already, and the results have come in have been very fruitful and promising.
Quoted further…
“In 2 reports, experiments on humans [16,17] involving the intraarticular injection of autologous MSCs yielded good results after 6 months. In 2008, Centeno and colleagues reported the use of autologous culture-expanded bone marrow- derived stem cells for knee cartilage regeneration in humans [17]. In their study, the patients’ pain, as determined by the VAS, and range of motion improved, and MRI showed significant articular cartilage growth and meniscus regeneration. “
What I personally got out of it…
I learned that the source of where you get the MSCs is quite important. While it is well known that MSCs can be filtered from bone marrow, bone marrow extractions are often very painful and have a high chance for infections and complications. In addition, as a person ages, the density of MSCs decrease. That seems to be why the researchers here used the infrapatellar fat pad as the source of the stem cells. They were able to get 9.4 g of infrapatellar fat pad which gave out on average about 1.89×10^6 stem cells, which is a nice cell to overall fat density. For future references, instead of asking that we get stem cells from bone marrow biospys, it would be much easier and simpler to use the source of fat from under the patella.
The last important thing that the researchers stated in the study was this ….
“the paracrine effects of the cytokines and growth factors released by the grafted cells, which favorably influence the microenvironment by triggering host-associated signaling pathways and lead to increased angiogenesis, decreased apoptosis, and possibly, induction of endogenous generation”
I am still trying to understand what this part means and what the implications are.
