Restoring Lost Height From IVD Collapse Is Already Possible But What About Healthy Thick Discs?
 Ever since I put up the contact us button to the sidebar which is linked to our contact us web page the amount of messages and information that is reaching the website email has increased 5X. With most of the messages, the readers of the website have really found some amazing resources which prove some concepts which we suspected was being done already.
Ever since I put up the contact us button to the sidebar which is linked to our contact us web page the amount of messages and information that is reaching the website email has increased 5X. With most of the messages, the readers of the website have really found some amazing resources which prove some concepts which we suspected was being done already.
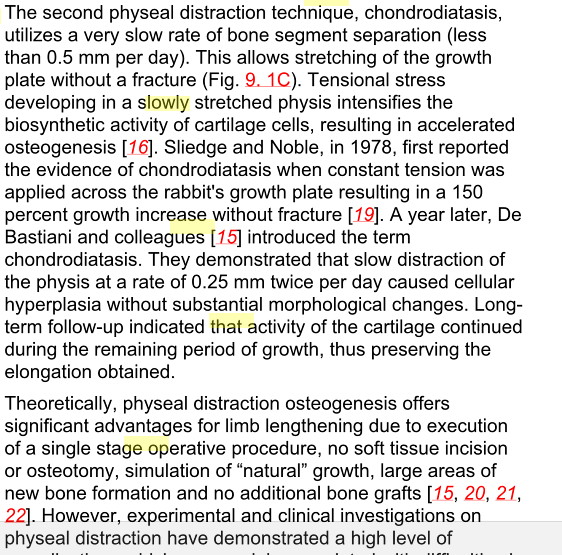
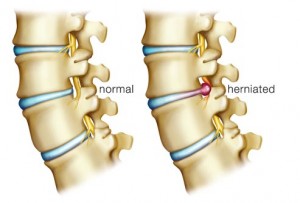
In the past, we’ve found multiple patent proposals on how it would be possible to restore the lost height people have after suffering something like a bulging disc or herniated or had their discs crushed by the amount of mass that on the upper torso of the body. We all know that over time, as people get older, they usually loss height. Having any type of medical condition which affects the back (or more specifically the lower back like the L4-L5 region) can make the height lost much greater.
I personally have read a few forum threads around the internet where people loss even upwards of 1.5-2 inches after developing a serious back problem like kyphosis, which is hunched back. Of course, it could be even worse than just 2 inches.
If their is a medical cause making the person loss height from disc degeneration, there are now multiple ways to treat that and restore height. I list the following articles and sources that the people who have messaged us have given us…
Source #1: New stem cell transplant holds promise for treatment of degenerative disc disease
Senior author, Wenchun Qu, MD, PhD, of the Mayo Clinic in Rochester, Minnesota – stem cell therapy for disc degenerative disease might be a potentially effective treatment…. not only did disc height increase, but stem cell transplant also increased disc water content and improved appropriate gene expression…. prepare for translation of stem cell therapy for degenerative disc disease into clinical trials….The increase in disc height was due to restoration in the transplant group of the nucleus pulposus structure, which refers to the jelly-like substance in the disc, and an increased amount of water content, which is critical for the appropriate function of the disc as a cushion for the spinal column, the researchers concluded.
Source #2: Intervertebral disc regeneration in an ex vivo culture system using mesenchymal stem cells and platelet-rich plasma
Here are excerpts of the abstract which we just copy and pasted below….
An ex vivo degenerative intervertebral disc (IVD) organ culture system… a stem cell and growth factor-based therapeutic approach for the amelioration of IVD.
…different therapeutic regimens including: (1) mesenchymal stem cell derived from eGFP-transgenic porcine (MSC-GFP), (2) platelet-rich plasma (PRP) and (3) MSC-GFP/PRP combined treatment, and confirmed in in vivo animal model…. Col II and aggrecan were found upregulated and chondrogenic matrix deposition increased…
PRP that has been shown to promote nucleus pulposus (NP) regeneration also resulted in significant increased levels of mRNA involved in chondrogenesis and matrices accumulation…. repeated and supported by in vivo porcine degenerative system.
Moreover, the disc height index (DHI) was significantly increased in both in vivo MSC-GFP and PRP regeneration groups
Source #3: Molecular and genetic advances in the regeneration of the intervertebral disc
Rapid advances… have resulted in several promising methods to facilitate the translation of laboratory-based techniques to clinical disc regeneration…. Tissue engineering strategies that employ (1) biomimetic scaffold materials, (2) differentiation-driving bioactive molecules, and (3) multipotent cells to enhance disc regeneration are being developed at a rapid pace.
The paper was not one of those papers written to say something new, but to organize all the possible ways that the current medical community knows how to restore the discs. Here was a list of the ideas that tissue engineering researchers around the world have tried…
1st Approach: Disc Regeneration Via Morphogens and Mitogens
- Delivery of exogenous proteins: Growth factors and cytokines
- Factors with biologic activity: Mitogens, morphogens, and intracellular mediators (ex. TGF-Beta1, TGF-Beta3, IGF-1, etc)
- Transforming growth factor beta superfamily; morphogens and biologic mediators of intravertebral disc development
- In-vitro (and In-Vivo) study of BMP-2 for IVD regeneration
- BMP-7 (aka OP-1) induces similar in vitro effects as BMP-2 in IVD cells
- In vitro and in vivo studies of BMP-14 (GDF-5)
- More work is needed to ascertain effects of lesser known bone morphogenetic proteins family members (like BMP-4 and BMP-13)
2nd Approach: Cell-Based Regenerative Strategies
- MCSs
- MCSs from bone marrow which can differentiate into nucleus pulposus like phenotype
- In vivo experimentation demonstrates the promise of marrow-derived mesenchymal stem cells
- Multiple niches of mesenchymal stem cells display regenerative properties
3rd Approach: Intervertebral Disc-Derived Cells
- Cells derived from intervertebral disc… rejuvenate endogenous cells
- Notochordal cells
4th Approach: Advances in Gene Therapy and Delivery
- Altering genotype of cell population, transcription/translation sustains protein synthesis
- Direct in vivo gene therapy: Direct administration of infecting agent(s) to host
- Adenoviral vectors expressing numerous bone morphogenetic proteins
- Sox9 gene delivery in human IVD cells
- Primary human IVD cells respond favorably to adenoviral infection with growth factors
- Treatment of IVD cells with lim mineralization protein-1 causes increased production of proteoglycans both in vitro and in vivo
5th Approach: Multi-Faceted Approaches to Disc Regeneration
- In vivo performance of cell-seeded scaffolds
6th Approach: Hydrogel-Based Scaffolds: A Promising Method for Nucleus Regeneration
- In vivo growth factor delivery from scaffolds
7th Approach: Enhancing Disc Regeneration by Slowing The Degenerative Process
- Proteinase inhibitors utilized in gene therapy-based approaches
- Statins act as intracellular inhibitors of MMP production and enhance BMP-2 mRNA expression
- Lactoferricin causes increased PG accumulation and downregulated catabolic processes
- TNFα-stimulated gene product TSG-6 with inter-α-inhibitor downregulate MMP activation
- Etanercept is an approved TNF-α inhibitor
- The oral administration of CPA-926 an esculetin prodrug
Source #3: Duke Bioengineers Develop New Approach to Regenerate Back Discs
In a proof-of-concept study published online in the journal Biomaterials… a new biomaterial designed to deliver a booster shot of reparative cells to the nucleus pulposus, or NP — the jelly-like cushion naturally found between spinal discs. The NP tissue distributes pressure and provides spine mobility, helping to relieve back pain.
- Primary Goal: “Our primary goal was to create a material that would be liquid at the start, gel after injection in the disc space and keep the cells in the location where they’re needed,”
- Secondary Goal: “Our second goal was to create a material that would provide the delivered cells with the environmental cues to promote their persistence and biosynthesis.”
The most common types of problems: …re-implanting NP cells, or even stem cells, can delay disc degeneration. Several companies already offer cell delivery strategies, but the methods are poor and ineffective. (using the currently available cellular delivery strategies, 100 percent of the injected NP cells leak out of an IVD site within three to four days after injection. ) “They allow the cells to quickly migrate out of and away from the injection site,” Francisco said.
The Duke team’s delivery strategy keeps the cells in place and provides cues that mimic laminin, a protein in native nucleus pulposus tissue. Laminin is normally found in juvenile but not degenerated discs and allows injected cells to attach and remain in place with the delivered biomaterial. Laminin may also enable the cells to survive longer and produce more of the appropriate extracellular matrix or structural underpinning of the discs that help stop degeneration, Setton said.
The researchers… developed a gel mix designed to reintroduce NP cells to the intervertebral disc (IVD) site. The gel mixes together three components:
- the protein laminin-111 that has been chemically modified
- two polyethylene glycol (PEG) hydrogels that can attach to the modified laminin.
Separately, these substances remain in a liquid state. The gel, however, holds the cells in place upon injection.
What they did: ….injected the gel into rats’ tails… puncturing the tail’s thin outer layer, they held the needle in place for one minute, delivered the injection to the rat’s IVD site, and closed the injection spot. The solution began to solidify after five minutes and was completely set at 20 minutes.
The Result: …more than 14 days after injection significantly more cells remained in place when delivered within the biomaterial carrier compared to cells delivered in a liquid suspension.
“The concept is that these cells will be promoted to produce matrix that can support tissue regeneration or arrest degeneration,” Setton said….
The exact study that the article above refers to is “Injectable laminin-functionalized hydrogel for nucleus pulposus regeneration.“
Source #4: NOVOCART® DISC
is a high-quality autologous cell compound in an innovative hydrogel for the biological reconstruction of partially damaged discs following disc prolapse
Biological disc reconstruction
…biological reconstruction of partially damaged disc tissue before massive degeneration… transplantation of in vitro cultivated chondrocytes from autologous disc tissue,or ADCT (Autologous Disc Cell Transplantation).
ADCT is comparable to joint ACT (Autologous Chondrocyte Transplantation)… In both cases, isolated from the biopsy material, the cultivated cartilage cells induced the desired reconstruction.
One further special feature…is the hydrogel used, which fixes the cells in the damaged disc… also anti-inflammatory.
Description of ADCT with NOVOCART® DISC
Transplantation of the cultivated disc cells can take place three months after extraction by way of operation of the prolapsed disc. The relatively long period between tissue extraction and cell transplantation must be adhered to, to ensure that the protective fiber ring (annulus fibrosus) is fully healed following the intervention.
So what do these 4 sources which was sent to us suggest?
We know that there are at least 2 different research teams at universities which are doing research to figure out how to restore the function and shape of IVDs after they have suffered through discs degeneration, whether due to just normal old age or some type of degenerative disease.
Since these teams are able using whatever technique to restore the shape of the IVD, they have also increased the thickness, which translates to mean that the person regained lost height.
Whether it is a scaffold implant, or cells like MSCs, or growth factors, the discs can be saved and given new life.
The first point is this – We now have multiple options on how to restore lost height from the collapse of the IVDs.
However, can we do anything if the discs are healthy and we want to increase our height?
I suspect that for most people, we are not fully maximized on how tall we can be. The majority of people would be able to gain upwards of even 1.25 inches in extra height, if we can correct our posture, and then our IVD structural integrity. If we wanted to, we could use these developing technologies to make sure that our nucleus pulposus matrix is strong and rich in the right collagen material.
However, there are a small group of people who have the discs already full. Maybe we are 18-20, with a completely healthy body but our only problem is that we suffer from familial short stature. For these people, who have already done all the stretching, the disc decompressions, and maybe tried even certain traction machines, I would suggest that we would no longer focus on the discs, but to focus on the material next to the discs.
However, the problem is probably going to have more to do with medical ethics than a technical problem. Most doctors would never agree to sticky a needle into the spinal area of a healthy young adult. There is a great fear that a needle stuck in the wrong area would cause a disc to become punctured or even slight paralysis.
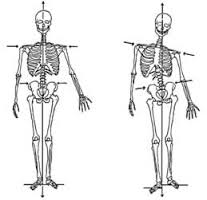
In a rather old post I did, it was shown that for young adults, around the 17-23 range, many of them have a very thin layer of articular cartilage that does run between the bone tissue of the vertebrate bone and the nucleus pulposus of the discs. That layer of cartilage however is so thin that it is very hard to see. It was guessed that the layer is most likely about 1-2 mm thick. However, we can work with that.
If might be possible to stimulate that layer of articular cartilage to go through hypertrophy using a small injection of IGF-1 directly into the cartilage tissue. We know that a local injection of IGF-1 into the bone layer under the periosteum would increase the rate of long bone longitudinal growth, as we had revealed in a previous post “Increase Height And Grow Taller Using Local Subperiosteal Injection Of Growth Factors IGF-1 And TGF-Beta Percutaneously” as long as the epiphyseal growth plate cartilage was intact.
Since the young adult who wants to grow taller, but has full discs, still has maybe 1-2 milimeter of cartilage in every connecting segment between the discs and the vertebrate bone, it should be reasonable to inject the IGF-1 (or TGF-Beta) locally next to the layer of thin articular cartilage. Since there is 33 vertebrate bones in the human skeletal system, we probably have 20 or so thin layer of cartilage we can try to stimulate using small needles.
If we can use an X-ray to double check the location of the needle injections, to make sure that we don’t puncture a disc or hit a nerve ending, it could work. The hypertrophic effect of injections of the growth factor into 20 of these thin layers can add up to maybe 2-3 extra inches, but that is a very wildly optimistic situation.
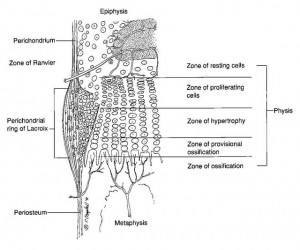
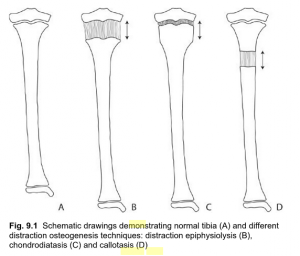 For a long time I’ve wondered whether it was possible to do more than just stretch out the bone tissue to make the overall bones longer, and it seems that there have been a few recent articles which came out showing that it is indeed possible to stretch out cartilage (epiphyseal growth plate) tissue. More than just stretching the cartilage, it seems that it would not even result in any type of fractures.
For a long time I’ve wondered whether it was possible to do more than just stretch out the bone tissue to make the overall bones longer, and it seems that there have been a few recent articles which came out showing that it is indeed possible to stretch out cartilage (epiphyseal growth plate) tissue. More than just stretching the cartilage, it seems that it would not even result in any type of fractures.