Understanding deformation will understand how to help grow taller as bone lengthening is a form of bone deformation. The problem with tensile(stretching) loading of bone is that it’s plastic so it’ll bounce back to it’s original length. It’s also hard to generate enough force to stretch bone.
Material heterogeneity in cancellous bone promotes deformation recovery after mechanical failure.
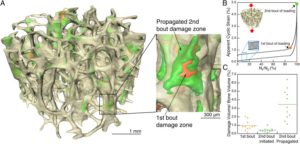
“Many natural structures use a foam core and solid outer shell to achieve high strength and stiffness with relatively small amounts of mass. Biological foams, however, must also resist crack growth. The process of crack propagation within the struts of a foam is not well understood and is complicated by the foam microstructure. in cancellous bone, the foam-like component of whole bones, damage propagation during cyclic loading is dictated not by local tissue stresses but by heterogeneity of material properties associated with increased ductility of strut surfaces. The increase in surface ductility is unexpected because it is the opposite pattern generated by surface treatments to increase fatigue life in man-made materials, which often result in reduced surface ductility. the more ductile surfaces of cancellous bone are a result of reduced accumulation of advanced glycation end products compared with the strut interior. Damage is therefore likely to accumulate in strut centers making cancellous bone more tolerant of stress concentrations at strut surfaces. Hence, the structure is able to recover more deformation after failure and return to a closer approximation of its original shape{we would not want this in terms lf lengthening bone, we don’t bone to return to it’s original shape we want it to be longer}. Increased recovery of deformation is a passive mechanism seen in biology for setting a broken bone that allows for a better approximation of initial shape during healing processes and is likely the most important mechanical function. Our findings suggest a previously unidentified biomimetic design strategy in which tissue level material heterogeneity in foams can be used to improve deformation recovery after failure.”
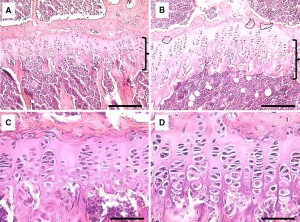
“Whole bones consist of a dense shell of cortical bone surrounding a foam-like tissue called cancellous bone. Bone tissue itself is a hierarchical composite consisting of a mineral component (primarily impure hydroxyapatite) and an organic polymer component (primarily type I collagen).”
“Completed remodeling sites have highly mineralized boundaries known as cement lines that contribute to crack deflection, thereby increasing tissue toughness”
Here’s an image showing what microcracks look like in trabecular bone although to get bone length you’d to cause microcracks in cortical bone:
“the presence of a more ductile strut surface forces tissue damage and associated permanent deformations into strut centers.”
“On unloading, struts that accumulate tissue damage in the center (where stresses are lower) will recover more deformation from bending and torsion than struts accumulating damage at surfaces.”
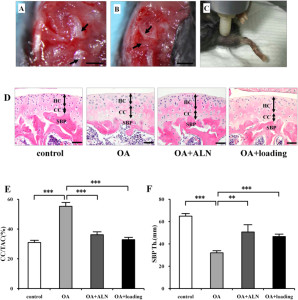
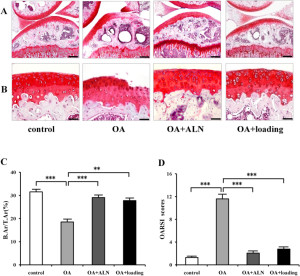
Here’s a paper that shows plastic deformation:
Acute plastic deformation of the ulna in a skeletally mature individual
“Acute plastic deformation of a bone refers to traumatic bending or bowing without a detectable cortical defect{we don’t want bending or bowing we want longitudinal stretching but this shows that plastic deformation is possible}. We present a case that is unusual in that bowing of the ulna occurred in a skeletally mature individual and was associated with injury to the distal radioulnar joint. In this patient, the symptoms were severe enough to warrant an ulnar osteotomy. The patient regained satisfactory function. Acute plastic deformity should be suspected whenerver abnormal curvature of a long bone is noted, even in adults. If the distal radioulnar joint is dislocated, the deformation should be corrected as soon as possible to avoid permanent loss of forearm rotation.”
Couldn’t get the full study but just the abstract is pretty much a breakthrough because it proves that plastic deformation is possible in a skeletally mature individual. But longitudinal plastic deformation is very difficult.