I will be going over all the LSJL studies to see if I missed anything or to find new insights.
Osteogenic potentials with joint-loading modality.
Here’s the paper: osteogenic LSJL study.
“Osteogenic potentials with a novel joint-loading modality were examined, using mouse ulnae as a model system. Load-induced deformation of rigid bone [generates] interstitial fluid flow and stimulate osteogenesis. However, in most of the previous studies, loads were applied to cortical bone. In the current study, we addressed the question of whether deformation of the epiphysis underneath the joint would enhance bone formation in the epiphysis{New bone formation in the epiphysis can increase height if the bone is added at the longitudinal ends} and the diaphysis. We applied lateral loads to a mouse elbow. Compared to the no-loading control, 0.5-N loads, applied to the elbow at 2 Hz for 3 min/day for 3 consecutive days, increased the mineralizing surface (two- to threefold), the rate of mineral apposition (three- to fivefold), and the rate of bone formation (six- to eightfold) in the ulna. Strain measurements indicated that strains of around 30 microstrain{30 microstrain is extremely low according to mechanostat theory}, induced with the joint-loading modality, were under the minimum effective strain of around 1000 microstrain, which is considered necessary to achieve strain-driven bone formation. To evaluate the induction of fluid flow with the joint-loading modality, streaming potentials were measured in separate experiments, using mouse femurs ex vivo. The streaming potentials correlated to the magnitude of the load applied to the epiphysis, as well as the flow speed in the medullary cavity. Joint-loading [induces] osteogenesis, through a mechanism that involves the induction of fluid flow in cortical bone.”
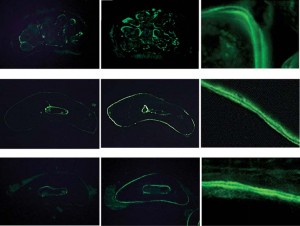 Column 1 is unloaded. Column 2 and 3 is LSJL loaded. It’s hard to tell in this pictures if LSJL created any gaps in the bone where new growth plates could form. The diagrams are not in enough to tell to notice the formation of any microgrowth plates at least in figure 2a. Calcein staining was used in these studies which detects mostly Ca2+ and Mg+ so it cannot distinguish between potential micro-growth plates and regular bone.
Column 1 is unloaded. Column 2 and 3 is LSJL loaded. It’s hard to tell in this pictures if LSJL created any gaps in the bone where new growth plates could form. The diagrams are not in enough to tell to notice the formation of any microgrowth plates at least in figure 2a. Calcein staining was used in these studies which detects mostly Ca2+ and Mg+ so it cannot distinguish between potential micro-growth plates and regular bone.
Here’s what the text had to say about the above diagram:
“Cross-sections of the ulnar shafts of control (no loading) and joint-loaded mice. The zoom images on the far right show double calcein staining, where the confined area constituted bone newly formed in 4 days. A Section of the metaphysis (trabecular bone) 1 mm from the loading center. The light staining outside the periosteal surface is collagen autofluorescence in a tendon of the triceps. B Section of the diaphysis (cortical bone) 2.5 mm from the loading center. C Section of the diaphysis (cortical bone) 4.5mm from the loading center”
“Trabecular bone in the epiphysis is less stiff in the lateral direction than in the axial direction and, therefore, lateral loads to the elbow may effectively deform the epiphysis of the ulna.
Deformation of the epiphysis may then induce fluid flow in the ulnar diaphysis in cortical bone, and load-induced fluid flow may enhance bone formation in the epiphysis{and possible stimulations of the epiphysis could be such as to spur new longitudinal bone growth} and the diaphysis.”
14 week old mice were used. “3min per day for 3 consecutive days. The loading force was sinusoidal, at 2Hz, with a peak-to-peak amplitude of 0.5N.”
“The measured intramedullary streaming potential (f1, in mV) correlated to the magnitude of the applied force, according to the equation: f1 = 7.3 ¥ F (r2 = 0.92)”
“the magnitude of the streaming potential in the medullary cavity is proportional to the lateral load applied to the joint and the speed of fluid flow.”
If you look at figure 1a you can see that the device used is a lot like a C-class clamp with the nylon screw.
“The tip of the loader had a contact area of 4 mm in diameter. In order to avoid local stress concentrations between a joint and the loader, the surface of the loader was covered with a silicon rubber sheet.”
It should be noted by analyzing Table 1 that LSJL increases the bone formation rate of bone near the periosteum than trabecular bone. Since the periosteum is partially involved in growth plate formation this is not necessarily a bad thing and since trabecular bone is still stimulated it still means that LSJL stimulates all areas of the bone and that LSJL could target any area of the bone that could be required to be targeted for neo-growth plate formation.
“[With axial loading], the force required to elevate the rate of bone formation is reported to be 2.3 N . With the joint loading modality described here, bone formation was enhanced by loads as small as 0.5 N.”<-So LSJL requires about 21% as much load to stimulate the bone as axial loading. Let’s say hypothetically, that 1000lbs of axial loading could stimulate neo-growth plate formation. LSJL would only require 210lbs. Although, the rate of bone formation is irrelevant to what we’re looking for as we’re looking for longitudinal bone formation via neo-growth plates and that may be a result of stimulus that is unique to LSJL that axial loading cannot provide.
“The cross-sectional images of the ulna, together with the data on bone strains, support the notion that enhanced formation of cortical bone was an adaptive response to mechanical stimuli rather than a response associated with wound healing. First, the histological sections clearly showed double-labeled staining on the periosteal surface, with no indication of woven bone, which would frequently be formed in the process of wound healing. Second, unlike the four-point bending modality, where woven bone is formed underneath soft connective tissues, due to bending moment or compressive stress”<-it may be better if LSJL did increase bone formation as a result of wound healing as that could indicate the formation of holes in the bone where neo-growth plates could form. However, the lack of woven bone could mean that cartilage was formed instead of bone which would be very promising indeed.
“the speed of the intramedullary fluid flow induced by 0.5-N loads, applied to the knee, is estimated as 476micro-m/s.”
This study was published in 2005 whereas lengthening of mouse hindlimbs with joint loading was published in 2010 so they were not yet aware of the lengthening effects. And the load was only applied for 3 days which is not a lot of time for bone lengthening to occur.
I did email the author to try get length data but I don’t know if he’ll respond.
